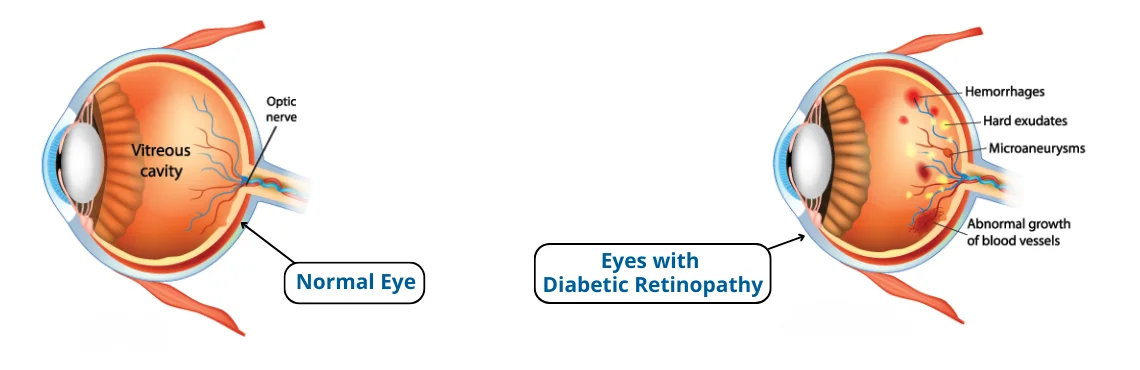
Diabetic Retinopathy (DR) is a serious eye condition associated with diabetes that occurs due to high levels of sugar in the blood, damaging small blood vessels that provide nourishment to the retina at the back of the eye. When damaged, these pipes can leak fluid or blood and make vision impaired - eventually rendering proper sight impossible.

Imagine your retina as being part of the eye that takes pictures and sends them directly to your brain, so you can clearly perceive what's around you. However, with this issue the picture may no longer be clear as intended: your vision might become blurrier, dark spots may float around randomly or colors may no longer look vibrant as before; some parts may even disappear entirely; shadows or gaps could appear where none existed previously.
Imagine it this way: your eyes are like cameras, with the retina serving as the film that captures images. When NPDR occurs, it's like some spots on that film get blurry; you might not notice at first but it's an early indicator that something's off behind the scenes.
Now here's the twist: just as you would stabilize a wobbly table leg with screws or glue, doctors can act to support blood vessels that may be weakening over time. They'll make sure everything doesn't deteriorate further while managing diabetes and getting regular eye check-ups can provide those wobbly bridges with extra support.
Remember, NPDR is like the opening chapter of a novel; by taking care of yourself and working closely with healthcare providers, you have the power to shape how the story progresses. By prioritizing wellness care for yourself and collaborating with healthcare teams on improving the future outlook for yourself.
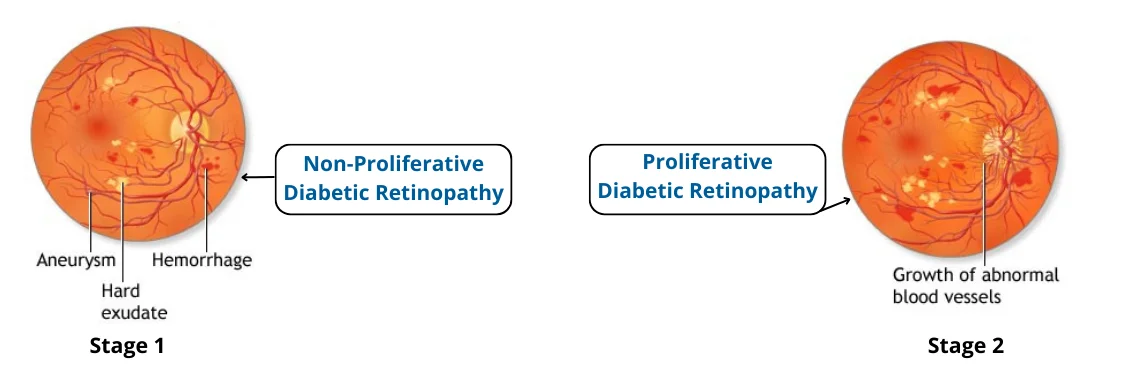
Imagine your eyes as an elaborate theater stage, with the retina as the central actor. PDR adds some new actors - small blood vessels that shouldn't be there but instead cause havoc by showing up unexpectedly and disrupting performance.
Imagine these vessels as thin threads, trying to be part of the scene but often becoming troublemakers. They might leak blood onto the scene or pull on the curtain (retina), leading it to tear apart.
Now here's the twist: just as in any play, a director must oversee everything and manage events accordingly. Doctors step in to make sure these new vessels don't create too much chaos and may use tools such as lasers to fix any scenes that become disordered and prevent further chaos from spreading.
But here's the good news: you aren't just watching this drama unfold; you are an active participant! By taking care to manage your diabetes, working with healthcare team, and getting regular eye checks-ups, you become the hero who helps maintain control over it all and help ensure this chapter doesn't overshadow overall eye health story.

| Aspect | Diabetic Retinopathy | Normal Aging Vision Changes |
|---|---|---|
| Cause | Related to diabetes and high blood sugar levels. | Part of the natural aging process. |
| Vision Blurriness | Gradual blurriness, often affecting both eyes. | Slow, gradual blurriness, usually in both eyes. |
| Vision Fluctuations | Vision may fluctuate throughout the day. | Consistent blurriness that worsens over time. |
| Floaters and Spots | Floaters and dark spots in vision possible. | Occasional floaters are common. |
| Peripheral Vision | Loss of peripheral vision may occur. | Peripheral vision narrows but doesn't disappear. |
| Dark or Empty Areas | Dark or empty areas in vision can appear. | Less severe dark spots or areas in vision. |
| Pain or Discomfort | May not cause pain; discomfort rare. | Typically painless; mild discomfort may occur. |
| Impact on Vision | Can lead to severe vision loss if untreated. | Mild to moderate vision changes; not as severe. |
| Treatment | Various treatments available, including laser. | Generally managed with corrective lenses. |
| Risk Factors | Diabetes, poor blood sugar control. | Aging is the main risk factor. |
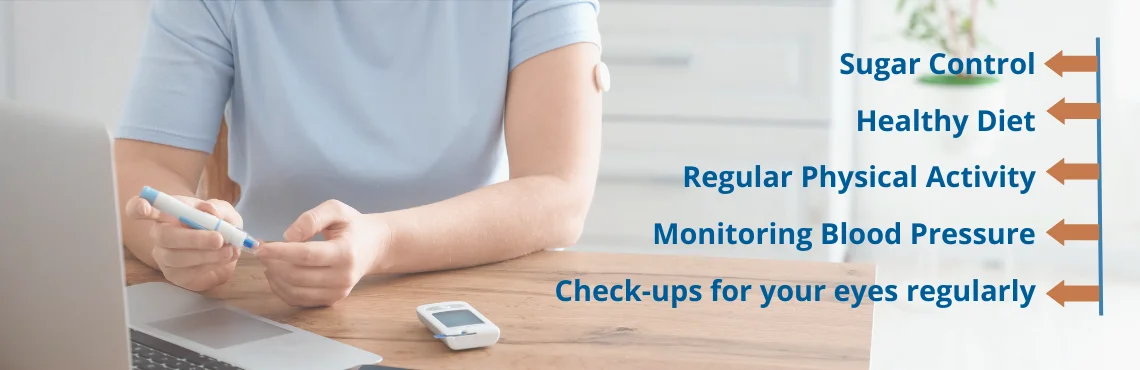
| Prevention | Control blood sugar, regular eye exams. | Regular eye exams, healthy lifestyle. |
Macular Edema can be treated with the following treatments:
Intra-Vitreal injections: Ophthalmologists work with numerous intravitreal injections to deliver medication to the eye's vitreous cavity. The underlying eye problem determines the injection and medicine. Common intravitreal injections are:
Anti-vascular endothelial growth factor (anti-VEGF) Injections:
Corticosteroid Injections:
Focal Grid Laser: Your ophthalmologist will burn retinal leaks around the macula with multiple tiny laser burns. Burns restrict fluid leakage and reduce retinal fluid. Focal laser therapy maintains eyesight. It halves eyesight loss risk. This treatment normally takes one session but may require more.
Both treatments are effective but do not cure this disease.
A comprehensive eye examination is crucial for the detection of this retinopathy and macular edema. This examination includes several tests:

If they find, macular edema or leaking blood vessels, additional tests may be performed:
These comprehensive eye examinations play a vital role in identifying and monitoring this type of retinopathy and macular edema. Regular screenings, along with appropriate treatment and management of diabetes, are essential for preserving vision and preventing complications.
Copyright © 2025 | Save Sight Centre | All Rights Reserved.